Good afternoon. Thank you for joining us today to learn how to best advocate for yourself and for your clients during the COVID-19 epidemic. My name is Kim Mcilnay. I’m a family physician, disabled from practicing medicine since 2009. In 2017, I started my patient advocacy practice, Together Patient Advocates, LLC. I love being able to combine my knowledge as a physician with my experiences as a patient to help improve the health of my clients.
I’m joined today by Caryn Cochran, a medical social worker who specializes in recovery from catastrophic illnesses and injuries. In her patient advocacy practice, Matters of Care, she helps patients and their families with benefits and resources, as well as psychological support and adjustment.
How can we as advocates best help our clients prepare for and manage the COVID-19 epidemic and the surrounding anxiety about the epidemic. We’ll discuss these issues over the course of this talk. I will post this video and a transcript to my blog on Together Patient Advocates. If you’re like me and you prefer to read, the full transcript of my talk is here. Please listen to Caryn's content as it is fantastic, but not fully transcribed (Her section starts at approximately 35 min). See below for her outline and for important links to further your study on the important techniques she shared.
If you’re not an advocate, but interested in learning more about COVID-19 and how to best prepare, we hope you find helpful tips here, too.
Neither of us are experts on COVID-19, but both of us have been researching this situation extensively in order to help our clients, and we feel it’s important to share what we know with our fellow advocates, so that you can better help your clients.
Please note, this talk should not be taken as medical advice, rather as information to help inform you about COVID-19. All medical questions should be directed to your physician. If you have follow-up questions please feel free to reach us via email: Kim@togetherpatientadvocates.com or Caryn@MattersofCare.org. We will try to answer your questions as soon as we are able. I, personally, have some medical issues that will limit my availability for responding. I’ll be taking breaks over the course of this recording as well. I apologize in advance for any recording “pauses” that aren’t seamless.
Please also note that the information regarding COVID-19 changes on a daily basis. Please see the list of resources at the end of the transcript for reliable sources through which you can stay most current. Some of the information covered today will be obsolete by tomorrow given how fast information is changing.
First, let’s establish a few basics:
COVID-19 stands for Coronavirus Disease 2019. Coronaviruses are NOT new. They are a group of viruses so named for crown-like spikes on their surface. There are many different types of coronaviruses that affect humans and/or animals and they typically cause respiratory illnesses, like the common cold. COVID-19 is a new type of Coronavirus which first appeared in Wuhan, China in December 2019. Coronaviruses mutate regularly (every year a new mutation causes us to come down with another cold), so we've anticipated for years that a new mutation could lead to an epidemic or a pandemic.As of March 9, 2020, at 9:45, according to the Johns Hopkins Interactive Map, COVID-19 spread to 109 countries and infected over 111,000 people, causing over 3,800 deaths. Within the US there are COVID-19 cases in 31 states with the coastal states being hardest hit. There are 545 cases with 21 deaths attributed to COVID-19.
We’re still trying to understand exactly how infectious and how deadly COVID-19 is:
- Reproductive Number: How contagious a virus is is measured by the reproductive number (R0, pronounced R naught). The R0 gives the expected number of secondary cases produced by a single infected person in a susceptible population. Currently, the R0 is believed to be between 2-3 (JAMA feb 27 update) meaning that for every one person infected, the infection is spread to 2 or 3 new people. In comparison, the Ro for influenza is 1.2.
- Case-Fatality Rate: The worldwide case-fatality rate of COVID-19 per the World Health Organization (WHO) on March 3, 2020 was 3.4%. It’s anticipated that this rate will decrease as more testing of mildly symptomatic patients is included. Indeed, with widespread testing, Korea is showing a case-fatality rate of less than 0.7%. Because of very limited testing abilities in the US at the present time, our case fatality rate appears to be very high, but we also know that we are missing many mildly symptomatic cases in that calculation which, if tested, would lower our rate. Many experts best estimates anticipate that the worldwide case fatality rate will land around 1% when this year is over.
- In comparison the case fatality rate for influenza is 0.1% and the R0 is 1.2.To put this into real numbers for our US population, influenza has already caused 32 million illnesses, 310,000 hospitalizations and 18,000 deaths during the current season in the US. If the case fatality rate of COVID-19 is indeed 1%, that results in 10 times as many deaths as we see from flu. We could then anticipate COVID-19 may cause 180,000 deaths in the US. The ultimate number of deaths will depend on how quickly this epidemic is controlled, how many “at risk” people acquire it, and what the true mortality rate ends up being. All of these are unknown at this point, with those numbers in reality being much higher or lower, depending on the true case fatality rate.
- It’s also important to note that mortality rates vary by age and comorbid conditions. The highest risk patients are over 60 or have serious underlying medical issues like heart disease, lung disease (asthma, COPD, etc), kidney disease, diabetes, immune deficiencies, obesity etc. This is important with regards to our clients as the vast majority of people who are hiring independent patient advocates are older and have serious underlying medical problems. In China, those 60-69 years old had a case fatality rate of 3.6%; 70-79 years old 8.0% and those over 80 years old had a case fatality rate of 14.8%.
- COVID-19 is a respiratory virus, transmitted through large droplets (droplets are the “spittle” you notice flying through the air when you cough or sneeze from a cold). There is some viral shedding through stool, so it is likely also spread through fecal-oral transmission.
- The incubation period (time from exposure to symptoms) ranges from 1-14 days per WHO and CDC.
- Symptoms most commonly include fever (83%-98% of patients), dry cough (76%-82%), and fatigue and myalgias (muscle aches) in 11%-44%.
- Less commonly reported symptoms include headache, sore throat, abdominal pain and diarrhea. There are misinformed posts circulating around social media citing runny nose and sore throat as presenting symptoms. This does not match the data from China or what we know thus far from US cases. Lack of a runny nose does not mean your cold symptoms are not COVID-19.
- Characteristic clinical findings include low white blood cell counts in 70%, bilateral patchy infiltrates on chest X-ray (though chest x ray can be normal earlier in the disease) and ground-glass infiltrates on chest CT. Chinese protocols included rapid chest CT scans of patients with possible COVID-19.
- At this time treatment is supportive care with oxygen supplementation as needed. There are studies underway to test various antiviral drugs, but thus far there is no proven treatment.
- In China, 80% of patients had mild disease, 15% required hospitalization and 5% of all cases were severe (meaning, they required intubation, were in shock, or had organ failure).
- No vaccine is available for COVID-19. It’s hoped that phase 1 vaccine trials will begin in Washington within the next 4 weeks. Keep in mind that if phase 1 studies show safety, phase 2 trial results would be available in 12-18 months and at that time we’ll know if the vaccine is even effective and safe. Widespread availability would be even longer away.
Why are US physicians so concerned about COVID-19?
- It’s a new virus. While we have the above estimates re rate of reproduction and mortality rates, these are just estimates.
- We don’t have great testing capabilities in the US at this time for a variety of reasons, including that early test kits were defective. We’re hoping that widespread testing will be available in the coming week, but we’re not certain if it will be. Thus, limited testing means we have limited numbers of cases currently. Note: if widespread testing is available in the next week, we can expect the number of confirmed cases to jump rapidly as a result of testing, not necessarily a sign of real-time rapid spread of the virus.
- Our hospitals are typically heavily impacted by patients with influenza and other respiratory viruses during the flu season, as they are at the current time. If we’re fortunate, and COVID-19 only hospitalizes as many patients as influenza, we will still have significant impacts on our hospitals and the ability of our medical staff to care for the increased number of patients, our availability of ER and hospital beds, ICU and isolation rooms and available ventilators. The data we have to date suggests COVID-19 will cause even more patients to be hospitalized than flu does; if that holds true, hospitals will be overwhelmed.
- As mentioned, we don’t yet have a vaccine or a known effective treatment.
- Our hospital and clinic supplies of personal protective supplies are extremely limited. I know physician and nurse colleagues who are having to ration their use of masks and gowns and are limited to one mask/day. This is simply just unacceptable. Unfortunately, the general public has stolen numerous supplies from hospitals and are also hoarding masks purchased over-the-counter.
- Quarantines of hospital staff, emergency responders, etc are impacting overall staffing levels and staffing levels will continue to worsen as healthcare workers either become sick from COVID-19 or are themselves quarantined. A recent exposure to a patient with COVID-19 at a major Sacramento hospital reportedly resulted in 124 staff out on quarantine, though the hospital disputes that. Another local hospital patient resulted in 10 staff and 3 EMS responders out on quarantine. You can see how this will quickly lead to serious staffing shortages.
- The medical staff I’ve spoken to and heard from feel unprepared for increasing numbers of patients and are not feeling strong support from our public health system in terms of being able to get necessary testing, supplies, or guidance re coordinated responses, etc.
- Lastly, in China, 3400 healthcare workers were ill with COVID-19 and at least 13 died. Our medical staff who are serving during this time understandably frightened about their own risks. Thus far, in the US, two physicians are reported to be ill with COVID-19.
Perspective: That was sobering, and perhaps anxiety inducing information about COVID-19. Let’s put this in perspective for a moment. Influenza is widespread in the community each year and infects 9-45 million annually in the US and kills 12,000-61,000 US patients yearly (CDC, Disease Burden of Influenza). Influenza this year is disproportionately affecting young children and young adults. Yet, the US population is not in a panic about flu every year and in fact, 50% of the US population REFUSES vaccines for a known, deadly disease. MUCH of the panic around COVID-19 in the population is related to it being new and unknown.
So, how can we prevent infection from COVID-19?
- Most simply, wash your hands with soap and water for 20 seconds, frequently. Twenty seconds is a long time - sing “Happy Birthday to You” all the way through twice or sing the ABCs all the way through once, including the invite "Next time won't you sing them with me, too". Turn off the water with a clean paper towel to avoid recontamination.
- Wash your hands frequently and always before and after eating, after sneezing or coughing, after leaving public areas, and when entering your home.
- See CDC handwashing guide for additional recommendations.
- This is a nice illustration of the effectiveness of different handwashing times. White shows bacteria left on hand. Source unknown.
- If soap/water is not available, use hand sanitizer that contains at least 60% alcohol. Use liberally and frequently.
- Avoid touching your face, eyes, nose and mouth.
- Use a tissue to cover a cough or sneeze and immediately dispose of the tissue and wash your hands.
- Clean frequently touched surfaces with usual household detergent and water per CDC. If disinfection is needed for known infection, use one of the COVID-19 approved disinfectants or a diluted bleach solution (realize it will ruin clothes/furniture). (https://www.americanchemistry.com/Novel-Coronavirus-Fighting-Products-List.pdf)
- If possible, telecommute. Many workplaces are offering telecommuting options and in person meetings have been cancelled and changed to web based meetings.
- Avoid sick contacts. Keep your distance from others and stay 6 feet away from others who are sick.
- Use hand sanitizer or wash your hands immediately on return home.
- Masks are not recommended for the general public at this time. Unfortunately, due to hoarding of masks, stealing of masks from clinics and hospitals, many are in short supply and medical staff are having to ration and re-use masks. These are the individuals who most need masks and who we as a society need to keep healthy so that they are able to take care of us when we’re sick. Many in public health believe that when the general population wears masks, it may actually increase their risk of infection due to more frequent face touching to adjust the mask. Regular surgical masks don’t protect the wearer from COVID-19 and N95 masks must be properly fit through a special procedure in order to protect from infection.
 Post on a friend's social media post from someone bragging that he'd "stocked up" when taking his friend to the ER!
Post on a friend's social media post from someone bragging that he'd "stocked up" when taking his friend to the ER! - Some schools are closed already. It’s advised to not allow your kids to hang out in groups with other children as a way of lessening spread through the community.
- Make use of live streaming to attend worship services virtually.
- And, of course, avoid sharing food and utensils.
- Avoid contact with “high touch” areas in public (elevator buttons, handrails, door handles, sink handles, etc.). When you must touch these areas, cover your hand with a tissue or your sleeve, use your knuckles, wrist, elbow.
-
Avoid crowds. This, unfortunately, means avoiding work conferences, movie theaters, pharmacies, etc. If you must be in a populated area, stay 3 feet away from others.
-
Reschedule elective medical appointments. For essential appointments, ask your doctor if the visit can be done via phone or video.
-
Avoid travel when possible. If you do plan to travel, evaluate the area you’re going to and be aware you could be stuck where you’re going, you could be quarantined on return home. If you yourself are in a high risk group, don’t go. If you’re in close contact with individuals in high risk groups, is it worth it to potentially infect them?
- Avoid handshakes, hugs, and kisses. Change your greeting to a wave, a foot shake, or some other salutation.
 (Source unknown, found on social media)
(Source unknown, found on social media)
Special Precautions for High Risk Individuals
- The CDC recommends that those who are over 60 or have severe chronic medical conditions (heart disease, lung disease (asthma, COPD, other), kidney disease, diabetes, immune deficiencies or are on medications that suppress the immune system, obesity) avoid leaving home as much as possible, avoid gatherings, travel, etc. This is a major change in lifestyle and will require support to make it possible. Perhaps healthy family members or neighbors can do your shopping for you, or you can have supplies delivered? Stock up before your community has widespread COVID-19 to lessen the need for more supplies. Have medications delivered via meds-by-mail or have someone else pick them up for you.
https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.htm
***** UPDATED LIST OF HIGH RISK CONDITIONS FROM CDC, 3/12/2020 ***- Blood disorders (e.g., sickle cell disease or on blood thinners)
- Chronic kidney disease as defined by your doctor. Patient has been told to avoid or reduce the dose of medications because
kidney disease, or is under treatment for kidney disease, including receiving dialysis - Chronic liver disease as defined by your doctor. (e.g., cirrhosis, chronic hepatitis) Patient has been told to avoid or reduce the
dose of medications because liver disease or is under treatment for liver disease. - Compromised immune system (immunosuppression) (e.g., seeing a doctor for cancer and treatment such as chemotherapy
or radiation, received an organ or bone marrow transplant, taking high doses of corticosteroids or other immunosuppressant
medications, HIV or AIDS) - Current or recent pregnancy in the last two weeks
- Endocrine disorders (e.g., diabetes mellitus)
- Metabolic disorders (such as inherited metabolic disorders and mitochondrial disorders)
- Heart disease (such as congenital heart disease, congestive heart failure and coronary artery disease).
- Lung disease including asthma or chronic obstructive pulmonary disease (chronic bronchitis or emphysema) or other chronic
conditions associated with impaired lung function or that require home oxygen - Neurological and neurologic and neurodevelopment conditions [including disorders of the brain, spinal cord, peripheral
nerve, and muscle such as cerebral palsy, epilepsy (seizure disorders), stroke, intellectual disability, moderate to severe
developmental delay, muscular dystrophy, or spinal cord injury. - When possible, if you are in a high-risk group, avoid contact with children. Children are NOT developing significant illness and many are asymptomatic, yet can still share COVID-19. It may not be possible to avoid contact given grandparents, for example, may be tasked to care for their grandkids while parents are working and schools are closed. In this event, avoid kissing/hugging/close contact and wash hands very frequently. If alternative child care is available use it.
* note: studies are showing hypertension as an independent high risk condition. See Lancet article.
Why try to lessen spread? We’re all going to get COVID-19 anyway, right?
- The goal is to lessen the immediate demand on the healthcare system. This chart is a nice illustration.
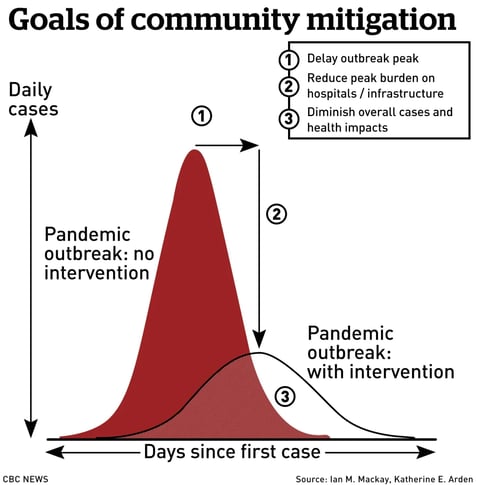
- If we don’t minimize contact, we can expect a large surge in sick patients all at once. This will overwhelm hospitals. If we’re able to limit community spread and slow down the rate of infection, we can expect a lower peak and the healthcare system will be better able to handle patients.
- Obviously, your approach if living in the Bay Area or NYC is going to be more urgent than if living in the middle of nowhere Ohio where there are no reported cases.
- Additionally, there is hope that spring/summer may lessen the virus, as it does with many respiratory viruses. However, we don’t know as this is new! Furthermore, typically these viruses return in the Fall, so we can anticipate needing to be ready in the Fall, if we are fortunate and it dies off over the summer. Slowing the spread throughout the community could lessen the total number infected right now and give us more time to prepare for next year.
- Data from China is very encouraging. The Chinese government responded swiftly to the outbreaks, tested widely and quarantined those who were sick. The rate of new infections has dropped significantly. If we can do similarly, our community as a whole will do much better.
How can we prepare for COVID-19?
- Have a one month supply of medications on hand at home. Some pharmacies are able to fill early or your physician may be able to write a justification for early refill. If unable to fill early, use meds-by-mail to have medications delivered when due, instead of going to the pharmacy where you’ll be exposed to multiple sick individuals. If unable to refill early through insurance, consider paying cash for extra medications through apps like GoodRx.
- Have a reasonable supply of medications you would need in event of a flu-like illness, for example your favorite cold medication, cough drops, etc. If you have asthma/COPD, ensure you have an adequate supply of albuterol. Have tissues on hand. In general respiratory illnesses, zinc lozenges have been shown to reduce the length and severity of illness. We don't know if they'll work the same way in COVID-19 but you may consider a short-term use of these WHEN symptoms start if ok’d by your doctor (longer term use can lead to other issues).
- A two to four week supply of food and living supplies is recommended. It is NOT necessary or helpful to hoard supplies. Everyone needs access to basic supplies. Recommended supplies include: easily prepared canned foods and vegetables, your usual “go to” sick day foods (soup, gatorade, whatever your personal comfort foods are), cleaning supplies (diluted bleach solutions recommended, vinegar water does not kill COVID 19).
If someone in your home becomes sick or is on quarantine:
- Stay home! Don’t expose the rest of the community to your illness.
- Designate a sick room/bathroom. The person on quarantine or who is sick should stay in that room only. If you must interact, the person who is sick should wear a mask and stay 6 feet away from others, Disinfect all surfaces frequently.
- Try to avoid going to the doctor unless necessary. If you are developing symptoms concerning for COVID-19, notify your doctor by phone or secure message. Most patients (80%) will have a mild illness and will be able to recover at home, without medical intervention. If you have symptoms that you are concerned may warrant a trip to the doctor, call your doctor’s office first for guidance and let them know you are concerned that you may have COVID-19 and what your symptoms are. Separate entrances into the clinic, or parking lot visits may be advised in order to prevent other patients from getting sick.
- Per the CDC, emergency COVID-19 symptoms in adults include
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face.
- *This list is not all inclusive. Please consult your medical provider for any other symptom that is severe or concerning.
- If you develop emergency warning signs for COVID-19 get medical attention immediately. If calling 911, notify them that you are concerned you have COVID-19 so that emergency responders can be adequately protected.
Now that we've reviewed all the basics re: COVID-19,
How can we best advocate for our clients?
- Review the above preparation and prevention steps with your clients. The CDC has easy to understand handouts on each topic.
- Arrange for community support (neighbors, friends, family) to coordinate trips to the store, pharmacy, etc for them so that they can stay home and avoid exposure.
- I’ve given each a copy of my medical care advocacy summary to my clients so that they have it available for emergency responders, ER/hospital. You can also assist those with smart phones to include this information in the medical alert sections of their phones so that it is available for them and for emergency responders, especially in event they are non-responsive on arrival. You can locate directions for doing this by googling “medical ID x phone.” I’ve posted two links below, but can’t verify the utility of the android link.
- Ensure you have signed informed consents to speak with medical staff for each of your clients. Many systems require your name to be listed in your client’s demographic section in the electronic medical chart. Now is the time to ensure that is done for each client.
- For those in nursing homes/assisted living, I encourage contacting administrators to determine what steps they are taking to prepare their residents for a COVID-19 outbreak. Areas to consider (these are my informed opinions, not direct guidance from CDC or public health) CDC Guidelines and CMS Guidelines.
- Signs on entry points to ask sick visitors to not enter
- Sick day policies encouraging ill medical staff to stay home when sick.
- Limit/prevent non-medical outings to avoid exposure to members sick in the community. Reschedule elective medical appointments.
- Disinfect high-touch areas frequently.
- Avoid community gatherings during an outbreak. Should there be someone at the nursing home who is infected with COVID-19, consider halting all group meals and activities Residents should have food brought to their rooms and limited interaction with staff as staff will be sources of transmission.
- Strict hand-washing by all staff before and after entering each room. Hand sanitizer outside and inside of each room and in high traffic areas.
- Plan for how to quarantine sick residents and how to care for them while avoiding transmission to other residents.
- Adequate medication and food supplies.
- Consider how you will best advocate for your clients should they require the emergency room or hospitalization during a community COVID-19 outbreak.
- You need to be listed in the demographics area of the hospital electronic chart so that staff can speak with you.
- Your client needs access to their medical summary and medication list.
- Your client needs to know to call you when interacting with staff so that you can hear the conversations, ask questions, etc.
- Anything your client comes into contact with needs to be disinfected with bleach containing wipes. This includes bed rails, TV remote, nurse call button, etc.
- All staff who enter the room to see your client should be
- Washing hands or using sanitizer on their way into the room and before examining your client.
- Sanitizing their stethoscopes before examining your client.
- Flu and Pneumonia Vaccines - Hopefully you’ve already advocated for your client’s health this fall and encouraged them to get their flu and pneumonia vaccines. If they refused at that time, or didn’t get around to it, this is the time to get it done. The flu vaccine is 40-60% effective this year, meaning that recipients may still get the flu, HOWEVER, those who have the vaccine will be MUCH less sick and at lower risk of complications if they receive the vaccine. This means, they will be less likely to need medical care/ER/hospital/ICU. This is one very practical way we can lessen the load on the medical system during the COVID-19 outbreak.
- Call their local pharmacies to ensure the vaccines are in stock.
- Clients should get the vaccines asap and go during a quieter time of day.
- Of course, if you haven’t received a flu vaccine, you need to as well.
- Determine how you will advocate for your clients should they become ill with COVID-19
- I personally am at higher risk of complications from COVID-19 due to underlying medical issues. Should my clients require hospital care, I will need to advocate for them remotely by phone/video. They are aware of this.
- You will need to make a decision as to how you will respond should a client require ER/hospitalization during COVID-19 community outbreak. Will you go to the ER? How will you protect yourself from infection while there (sit away from sick patients, frequent hand washing/sanitizer). If you will not be going to the ER/hospital to advocate for your clients, they need to know this now.
Reliable resources: There’s a lot of misinformation in the community. Where can you turn for reliable information? This list is NOT exhaustive, but here are some of the sites I’ve used to prepare this talk.
- CDC website
- Your state public health website.
- I’ve posted relevant, informative and quality articles on my work facebook page. You may wish to do the same to inform your clients and followers. I avoid posting dramatic, fear-based, word of mouth or politicized links on my work page.
- JAMA COVID updates
- ZDog COVID updates - generally reliable and fact-based, but based on one doctor’s experiences.
- Interactive Map from Johns Hopkins COVID-19
- WHO Situation Reports (updated daily)
- JAMA live interview with Dr. Anthony Fauci
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)
- Clinical Characteristics of Coronavirus Disease 2019 in China
- WHO hand sanitizer recipe
- Washington Post Corona Simulator - Fantastic visual simulation which highlights the importance of social distancing.
****
Managing Anxiety
by Caryn Cochran, Licensed Medical Social Worker
(Starts at 36:35 in above video)
So how do we help our clients -- and ourselves -- emotionally through this event?
First, it is normal to feel anxious, upset and worried – it is our mind’s response to perceived threats to keep us safe. It motivates us to pay attention and take action.
The issue is when worry and stress become chronic rather than temporary states that get us moving.
If we have a history of trauma, we are more quickly moved into fight, fight or freeze.
When we are responding from a place of trauma, our attention and focus are narrowed and our brain’s executive functions go offline. While this is effective in the moment, over the long haul it reduces our capacity to respond to a crisis in an effective, life-giving way.
How can we care for ourselves when we are in a place of worry and concern:
1. A daily meditation practice: https://nccih.nih.gov/health/meditation/overview.htm
2. Nourish your body with good sleep and good nutrition and your soul with good company: https://www.sleepfoundation.org/articles/how-does-anxiety-affect-sleep
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3762204/
https://www.healthline.com/health-news/stress-cues-from-others#4
3. Give yourself a worry budget: https://www.nytimes.com/2020/02/26/smarter-living/the-difference-between-worry-stress-and-anxiety.html
4. Get grounded in the here and now: https://www.healthline.com/health/grounding-techniques
5. Have a go-to gratitude list:
https://positivepsychology.com/neuroscience-of-gratitude/
6. Stay connected:
https://www.apa.org/monitor/2019/05/ce-corner-isolation



.gif?width=200&name=NAHAC-Member-Badge200x112+(1).gif)